Common Injuries: Plantar Fasciopathy
Plantar Fasciopathy
By Karl Kolbeck, PT, OCS, SCS, COMT, FAAOMPT
Rose City Physical Therapy
Often referenced as one of the top three running related injuries, plantar fasciopathy – commonly termed plantar fasciitis or plantar fasciosis – can be one of the most painful and limiting of running related injuries. It would be foolish to think this topic is new to you. Or to pontificate there exists an easy ‘fix’. There does not. Nor does a sound basis for treatment exist in the scientific literature; however, recent research provides insight into management strategies that are looking (cautiously) optimistic.
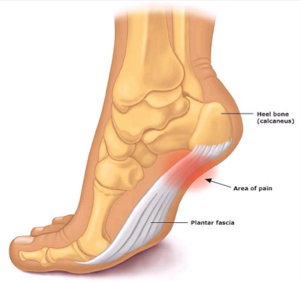 ‘-itis’...’-osis’...’-pathy’. Semantics, or purposeful? All three suffixes are derived of Greek origin: -itis meaning inflammation, -osis meaning abnormal condition, and -pathy meaning disease. Simply, upon initial injury or tissue breakdown - the acute phase – bleeding and inflammation occur. Studies of tissue samples at injury onset reveal a presence of inflammatory products; hence plantar fasciitis is defined. Approximately six to eight weeks after injury and beyond – the sub-acute and chronic phases – evidence of inflammatory infiltrate is negligible to nil. It’s at this time terminology appropriately shifts to plantar fasciosis. And of late the use of plantar fasciopathy is becoming more common, which essentially covers both aforementioned disease states.
‘-itis’...’-osis’...’-pathy’. Semantics, or purposeful? All three suffixes are derived of Greek origin: -itis meaning inflammation, -osis meaning abnormal condition, and -pathy meaning disease. Simply, upon initial injury or tissue breakdown - the acute phase – bleeding and inflammation occur. Studies of tissue samples at injury onset reveal a presence of inflammatory products; hence plantar fasciitis is defined. Approximately six to eight weeks after injury and beyond – the sub-acute and chronic phases – evidence of inflammatory infiltrate is negligible to nil. It’s at this time terminology appropriately shifts to plantar fasciosis. And of late the use of plantar fasciopathy is becoming more common, which essentially covers both aforementioned disease states.
The scope of this blog is not to blame glut amnesia – a weak or inhibited gluteal medius (lateral hip stabilizer) or gluteal maximus (the ‘crown’ jewel responsible for hip extension and terminal stance phase propulsion) – in spite of them currently being named the culprit for every lower extremity injury by the majority of personal trainers and rehab professionals. And if the gluts aren’t blamed, then the Iliotibial Band is labeled as culpable. There is no scientific evidence to support that a correlation between plantar fasciopathy and glut weakness and inhibition exists. The same goes for a tight ITB (which by the way research proves it cannot be stretched. [Falvey, 2010]).
Believe it or not, sometimes one can experience pain and dysfunction due to isolated stress and localized tissue or joint damage with all else adjacent firing on all cylinders. A comprehensive neuromusculoskeletal and biomechanical exam by a physical therapist experienced in orthopedic and sport injury can determine cause-effect relationships and establish an individualized plan of care. With this article focused on the runner, seeking a physical therapist that who also understands the specifics of the running gait cycle and corrective measures to foster healthy recovery would prove most valuable to you. For example, one recent article reported maximal force and force-time rates over the rearfoot and loading rates were significantly higher in runners with plantar fasciopathy [Ribeiro, 2015]. There are fundamental corrective procedures to address this.
 Recent research [Rathleff, 2014] compared a group using heel inserts and plantar fascia stretching to a group with heel inserts and high-load strength training. The high load strength-training group demonstrated superior self-reported outcomes after 3 months compared to the plantar-specific stretching group. The exercise has been shown promising for treatment and recovery from plantar fasciopathy. Its purpose, like eccentric loading for tendon pathology lesion, is to progressively load the plantar fascia and stimulate a healing response to increase the tensile properties of the tissue. Unique to this exercise is placing a rolled towel under your toes to maximally dorsiflex them.This places a pre-stretched load on the plantar fascia.
Recent research [Rathleff, 2014] compared a group using heel inserts and plantar fascia stretching to a group with heel inserts and high-load strength training. The high load strength-training group demonstrated superior self-reported outcomes after 3 months compared to the plantar-specific stretching group. The exercise has been shown promising for treatment and recovery from plantar fasciopathy. Its purpose, like eccentric loading for tendon pathology lesion, is to progressively load the plantar fascia and stimulate a healing response to increase the tensile properties of the tissue. Unique to this exercise is placing a rolled towel under your toes to maximally dorsiflex them.This places a pre-stretched load on the plantar fascia.
The protocol is performed every other day and consists of a slow 3-second single leg heel raise with towel roll under the toes followed by a 2-second isometric pause at the top of the heel raise, and then a slow 3-second eccentric lowering of the heel. Initially 3 sets of 12 reps are performed at body weight. At two weeks weight is added to a backpack and 3 sets of 10 reps are performed for two weeks. Thereafter, additional weight is added to the backpack and 4 sets of 8 reps are performed on the same every other day frequency.
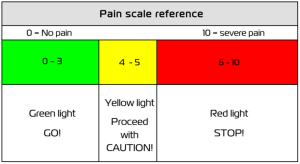 Proceed with caution if you attempt this exercise and your injury is recent. It’s likely not until the acute phase has passed that benefits of the high-load strength training will be appreciated. And a certain level of exercise ‘pain’ is expected and part of the protocol. I commonly allow patients to exercise through the 3/10 and perhaps into the 5/10 pain scale range. Coupled with other traditional management strategies this exercise has proven to be helpful with my chronic plantar fasciopathy patient caseload.
Proceed with caution if you attempt this exercise and your injury is recent. It’s likely not until the acute phase has passed that benefits of the high-load strength training will be appreciated. And a certain level of exercise ‘pain’ is expected and part of the protocol. I commonly allow patients to exercise through the 3/10 and perhaps into the 5/10 pain scale range. Coupled with other traditional management strategies this exercise has proven to be helpful with my chronic plantar fasciopathy patient caseload.

Karl Kolbeck is a physical therapist and along with his wife Sasha they own Rose City Physical Therapy located in NW Portland. He’s been practicing for 25 years with specialties in treating the shoulder as well as runners. Karl is dual board certified in both orthopedic and sports clinical specialties, is certified in manual and manipulative therapy and is a fellow of the American Academy of Orthopedic Manual Physical Therapists. He teaches rehab based continuing medical education courses to physicians, physical therapists and athletic trainers across the nation. He and his staff are involved with multiple running groups in the Portland metro area, offering educational sessions and athlete screenings. Karl also provides care for the Bowerman Track Club Nike professional running team based in Portland.
References:
- Falvey EC, Clark RA, Franklyn-Miller A, et al. Iliotibial band syndrome: an examination of the evidence behind a number of treatment options. Scand J Med Sci Sports. 2010 Aug;20(4):580–7
- Ribeiro AP, et al. Dynamic Patterns of Forces and Loading Rate in Runners with Unilateral Plantar Fasciitis: A Cross-Sectional Study. PLoS ONE 10(9) 2015
- Rathleff, MS. High-load strength training improves outcomes in patients with plantar fasciitis: A randomized controlled trail with 12-month follow-up: Scandinavian Journal of Medicine and Science in Sports. 2014
Connect With Us
see the latest from Fleet Feet PDX